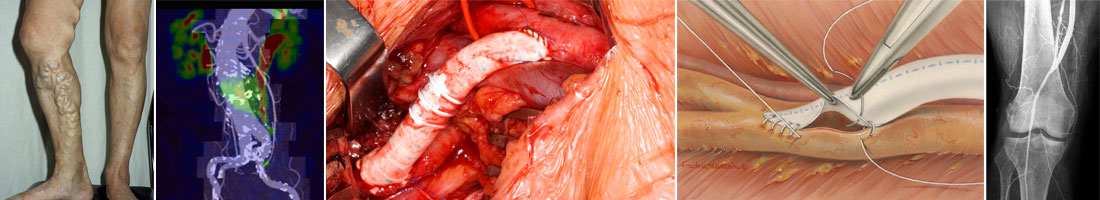
Both endartrectomy with patch plastic and bypass grafting are commonly used operative procedures to treat peripheral arterial occlusive disease.
During endartrectomy, the surgeon opens the artery and removes the atherosclerotic plaque together with the inner wall of the affected artery – hence the name “Endarterectomy”. Then the artery is closed using a patch (autologous vein, bovine pericardium, synthetic material) to increase the size of the lumen.
A vascular bypass is aimed at bridging an occluded arterial segment, redirecting blood flow from the vessel area with apparently normal blood flow to the vessel area without normal flow. For example, if a superficial femoral artery is occluded, then a bypass from a common femoral artery to a popliteal artery may be used.
The best graft material is an autologous vein, but if not available/suitable, synthetic materials (PTFE, Dacron) are used.
A narrowed/occluded segment of an artery may also be widened/opened using balloon dilatation – percutaneous transluminal angioplasty (PTA). For this purpose, through percutaneous access, a balloon catheter will be placed into the narrowed segment of the artery and the balloon will be inflated. Stent implantation during PTA procedure prevents possible re-stenosis of the dilated vessel, which may occur when the balloon is deflated and the catheter removed.
Although PTA is a low-risk procedure compared to surgery, potentially dangerous complications can occur. The most frequent complication is hematoma or pseudoaneurysm formation at the puncture site. If there are no complications, the patient can leave hospital the next day after PTA.
Limb salvage treatment allows the restoration of blood supply to an ischemic extremity suffering from circulatory disorders, which reduces the risk of major amputation.
For disease pattern see “Diseases”.